Abstract
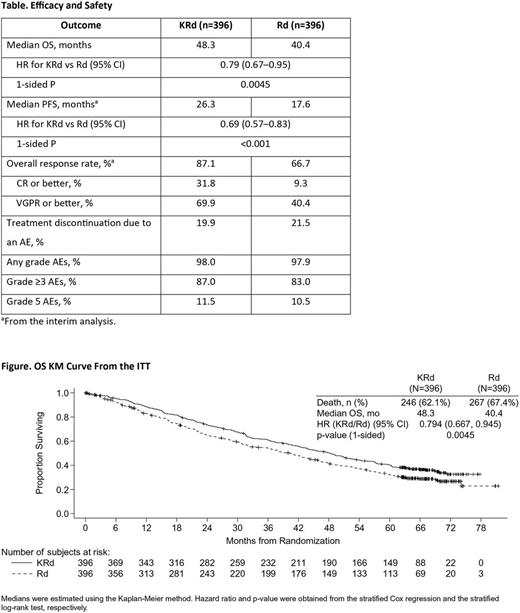
Background: The randomized phase 3 ASPIRE study demonstrated that the addition of the proteasome inhibitor carfilzomib to Rd resulted in significantly improved progression-free survival (PFS) compared with Rd alone in patients with RRMM (median 26.3 vs 17.6 months; hazard ratio [HR], 0.69; 95% confidence interval [CI], 0.57-0.83; 2-sided P=0.0001; Stewart AK, et al. N Engl J Med . 2015;372:142-52; Table). OS data were immature at the time of the PFS analysis but showed a trend in favor of the KRd group (HR=0.79). Hereby, results from the planned final analysis of OS in ASPIRE are presented.
Methods: Adults with RRMM who received 1─3 prior lines of therapy were eligible. Patients were randomized (1:1) to receive KRd or Rd in 28-day cycles until withdrawal of consent, disease progression, or the occurrence of unacceptable toxicity. Randomization was stratified according to β2-microglobulin level (<2.5 mg per liter vs. ≥2.5 mg per liter), previous therapy with bortezomib, and previous therapy with lenalidomide. Carfilzomib was given as a 10-minute infusion (starting dose of 20 mg/m2 on days 1 and 2 of cycle 1; target dose of 27 mg/m2 thereafter) on days 1, 2, 8, 9, 15, and 16 during cycles 1─12 and on days 1, 2, 15, and 16 (cycles 13─18). Lenalidomide (25 mg) was administered on days 1-21 and dexamethasone (40 mg) was administered on days 1, 8, 15, and 22. After cycle 18 of carfilzomib, patients randomized to the KRd arm received Rd treatment only. In total, 510 deaths were required to provide 85% power to detect a reduction in the risk of death for KRd vs Rd, with a 1-sided significance level of 0.025. OS was compared between treatment arms using a stratified log-rank test. HRs were estimated using a stratified Cox model.
Results: As of the data cutoff date (April 28, 2017) for the planned final OS analysis, median treatment durations were 72 weeks for carfilzomib (per protocol, carfilzomib was discontinued after cycle 18), 85 weeks (KRd arm) and 57 weeks (Rd arm) for lenalidomide, and 80 weeks (KRd arm) and 49 weeks (Rd arm) for dexamethasone. The median follow up was 67 months for both arms. Median OS (95% CI) was 48.3 (42.4-52.8) months for KRd vs 40.4 (33.6-44.4) months for Rd (HR, 0.79; 95% CI, 0.67-0.95; 1-sided P=0.0045; Table and Figure). Median OS was 11.4 months longer for KRd vs Rd in patients receiving 1 prior line (47.3 vs 35.9 months [HR, 0.81; 95% CI, 0.62-1.06]) and 6.5 months longer for patients receiving ≥2 prior lines (48.8 vs 42.3 months; [HR, 0.79; 95% CI, 0.62-0.99]). Among patients with 1 prior line of therapy, OS was improved with KRd vs Rd regardless of whether patients had received prior bortezomib; in patients with 1 prior line, median OS was improved by 12 months in the prior bortezomib group (45.9 vs 33.9 months [HR, 0.82; 95% CI, 0.56-1.19]) and 7.9 months in the no prior bortezomib group (48.3 vs 40.4 months [HR, 0.80; 95% CI, 0.55-1.17]). With respect to risk, OS by Revised International Staging System (R-ISS) stage was assessed. For R-ISS stage I (KRd, n=42; Rd, n=46), median OS was not reached for KRd and was 58.0 months for Rd (HR, 0.49; 95% CI, 0.26-0.92). For patients with R-ISS stage II (KRd, n=194; Rd, n=195), median OS was 45.4 months for KRd and 41.2 months for Rd (HR, 0.86; 95% CI, 0.68-1.10). For the small number of patients with R-ISS stage III (KRd, n=37; Rd, n=47), median OS was 23.3 months for KRd and 18.8 months for Rd (HR, 1.05; 95% CI, 0.66-1.68). For the overall study population, treatment discontinuation due to an adverse event (AE) occurred in 19.9% (KRd) and 21.5% (Rd) of patients. Fatal AEs were reported in 11.5% (KRd) and 10.5% (Rd) of patients. Grade ≥3 AE rates were 87.0% (KRd) and 83.0% (Rd). Selected grade ≥3 AEs of interest (grouped terms; KRd vs Rd) included acute renal failure (3.8% vs 3.3%), cardiac failure (4.3% vs 2.1%), ischemic heart disease (3.8% vs 2.3%), hypertension (6.4% vs 2.3%), and hematopoietic thrombocytopenia (20.2% vs 14.9%).
Conclusions: KRd demonstrated a statistically significant and clinically meaningful 21% reduction in the risk of death vs Rd. KRd should be considered a standard of care in RRMM.
Stewart: Celgene: Consultancy; Bristol-Myers Squibb: Consultancy; Janssen: Consultancy; Amgen: Consultancy; Roche: Consultancy. Siegel: Celgene, Takeda, Amgen Inc, Novartis and BMS: Consultancy, Speakers Bureau; Merck: Consultancy. Ludwig: Bristol-Meyers: Speakers Bureau; Celgene: Speakers Bureau; Janssen-Cilag: Consultancy, Speakers Bureau; Takeda: Consultancy, Research Funding, Speakers Bureau; AMGEN: Consultancy, Research Funding, Speakers Bureau; Takeda: Research Funding, Speakers Bureau. Facon: Amgen, Celgene: Speakers Bureau. Goldschmidt: Bristol-Myers Squibb: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Amgen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Chugai: Consultancy, Honoraria, Research Funding, Speakers Bureau; Takeda: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Millenium: Research Funding, Speakers Bureau; Novartis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Morphosys: Research Funding; Celgene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Janssen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Onyx: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Jakubowiak: Amgen Inc., BMS, Celgene, Janssen, Karypharm, Millennium-Takeda, Sanofi, SkylineDX: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; University of Chicago: Employment. San Miguel: Janssen: Consultancy, Membership on an entity's Board of Directors or advisory committees; MSD: Consultancy, Membership on an entity's Board of Directors or advisory committees; Amgen: Consultancy, Membership on an entity's Board of Directors or advisory committees; Bristol-Myers Squibb: Consultancy, Membership on an entity's Board of Directors or advisory committees; Sanofi: Consultancy, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees; Takeda: Consultancy, Membership on an entity's Board of Directors or advisory committees; Celgene: Consultancy, Membership on an entity's Board of Directors or advisory committees; Roche: Membership on an entity's Board of Directors or advisory committees. Obreja: Amgen: Employment, Equity Ownership. Blaedel: Amgen: Employment, Equity Ownership. Dimopoulos: Amgen Inc, Celgene Corporation, Janssen Biotech Inc, Onyx Pharmaceuticals, an Amgen subsidiary, Takeda Oncology: Consultancy, Honoraria, Other: Advisory Committee: Amgen Inc, Celgene Corporation, Janssen Biotech Inc, Onyx Pharmaceuticals, an Amgen subsidiary, Takeda Oncology; Genesis Pharma: Research Funding; Novartis: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.